

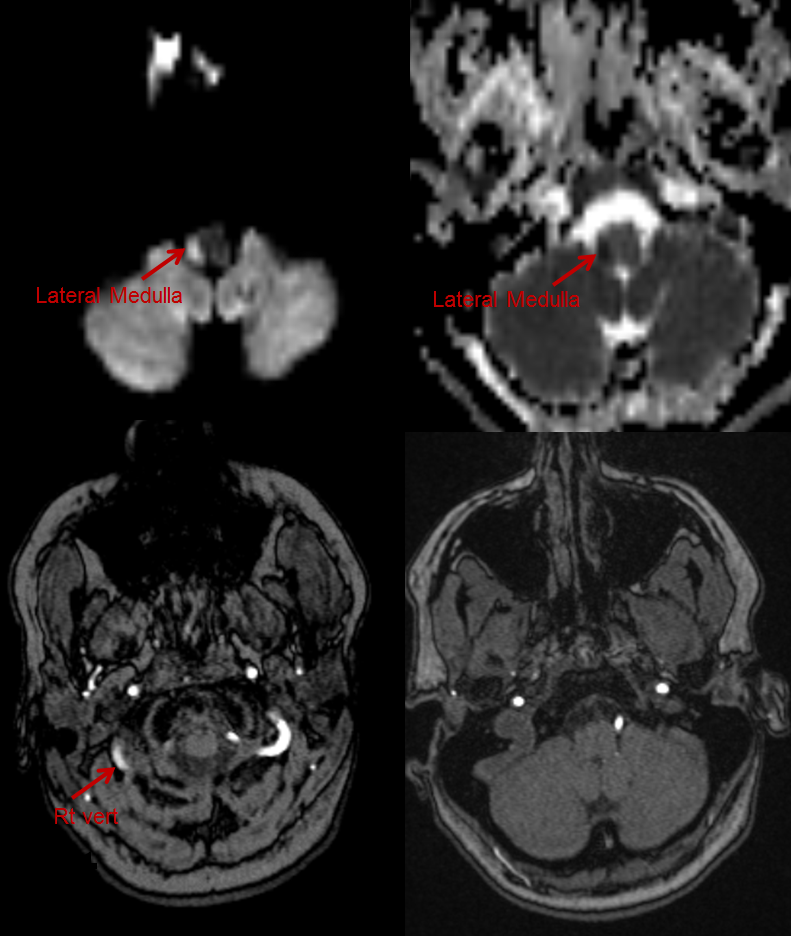
When the one vertebral artery responsible for supplying the major source of the blood flow is occluded, the resulting infarction is more severe than in the case of bilaterally competent vertebral arteries. 5 The relative sizes of the vertebral arteries vary considerably, and in approximately 10% of cases one vessel is so small that the other is essentially the only artery supplying the brainstem and cerebellum. Norrving and Cronqvist examined the pattern of vascular occlusion in lateral medullary infarctions, and found that the most common vascular lesions involved the vertebral arteries. The PICA and vertebral artery supply the lateral medullary area, and branches of the vertebral artery are distributed to practically the entire lateral medullary region between the medullary pyramids and the fasciculus cuneatus at the caudal medullary level. The arterial supply of the medulla arises from the vertebral artery, PICA, and anterior and posterior spinal arteries. 2, 3 In the present case, the lesion causing ipsilateral hemiparesis was located in the upper cervical cord, also involving the corticospinal tract below the decussation. Pathologic and neuroradiologic findings have identified the causal lesion of Opalski's syndrome. 1 He reported two patients with ipsilateral hemiplegia, ataxia, Horner syndrome, diminished facial sensation, and diminished superficial sensation of the contralateral side. Ipsilateral hemiparesis with symptoms and signs of lateral medullary infarction were first described by Opalski in 1946. MR angiography disclosed suspicious narrowing of the proximal and distal portions of the right vertebral artery and hypoplasia of the left vertebral artery ( Fig. Diffusion-weighted and T2-weighted brain MRI performed 24 hours after the onset of his condition revealed a high-intensity area in the right lateral medulla extending from the rostral medulla to the upper cervical cord, and in the right cerebellum in the territory of the medial branch of the posterior inferior cerebellar artery (PICA) ( Fig. During the next 7 days, his tone returned, the deep tendon reflex increased, and he developed a right-side Babinski response. On the second day in hospital, his right side became hemiplegic (upper/lower, II/II) with flaccid tone and hyporeflexia. Position and vibration senses were also decreased on the right side of his body. On sensory examination, pinprick and temperature sensations were decreased on the right side of his face and the left side of his body. On examination, his pulse was regular, his blood pressure was 160/100 mmHg, and his temperature and respiratory rate were normal.Ī neurological examination revealed right-sided hemiparesis (MRC grade: upper/lower, IV/IV), right Horner syndrome, and ataxia of his right limbs. The patient regularly took amlodipine besylate (5 mg once a day) for his blood pressure, but nothing for his diabetes.
A 64-year-old male was admitted with sudden onset of right-sided hemiparesis, headache, gait disturbance, and recurrent vomiting.


 0 kommentar(er)
0 kommentar(er)
